Spondylolisthesis / Spondylitis
Spondylolisthesis (spon + dee + lo + lis + thee + sis) is a condition of the spine whereby one of the vertebra slips forward or backward in relation to the next vertebra. Forward slippage of an upper vertebra on a lower vertebra is referred to as
anterolisthesis, while backward slippage is referred to as retrolisthesis. Spondylolisthesis can lead to a deformity of the spine as well as a narrowing of the spinal canal (central spinal stenosis) or compression of the exiting nerve roots (foraminal stenosis). Spondylolisthesis is most common in the low back (lumbar spine) but can also occur in the mid to upper back (thoracic spine) and neck (cervical spine).
Dr. Yash Shah is one of the best doctor for Spondylolisthesis treatment in Kandivali, Mumbai who provides effective solutions for Spondylolisthesis. Consult Now!
What causes spondylolisthesis?
There are five major types of lumbar spondylolisthesis.
● Dysplastic spondylolisthesis: Dysplastic spondylolisthesis is caused by a defect in the formation of part of the vertebra called the facet that allows it to slip forward. This is a condition that a patient is born with (congenital).
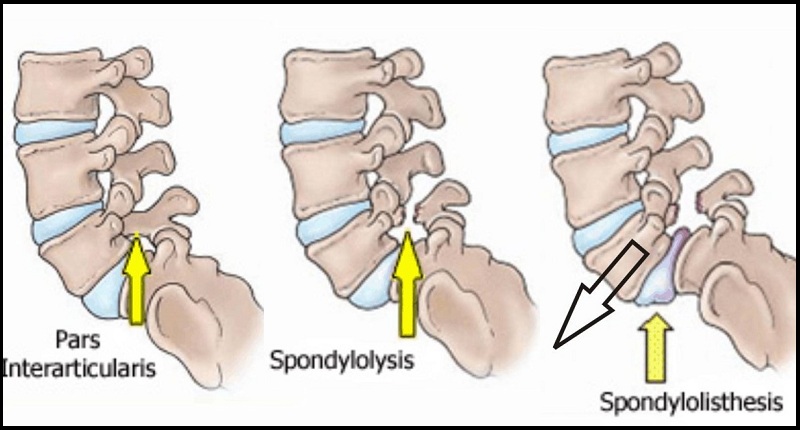
● Isthmic spondylolisthesis: In isthmic spondylolisthesis, there is a defect in a portion of the vertebra called the pars interarticularis. If there is a defect without a slip, the condition is called spondylolysis. Isthmic spondylolisthesis can be caused by repetitive trauma and is more common in athletes exposed to hyperextension motions, including gymnasts and football linemen.
● Degenerative spondylolisthesis: Degenerative spondylolisthesis occurs due to arthritic changes in the joints of the vertebrae due to cartilage degeneration and is acquired later in life. Degenerative spondylolisthesis is more common in older patients.
● Traumatic spondylolisthesis: Traumatic spondylolisthesis is due to direct trauma or injury to the vertebrae. This can be caused by a fracture of the pedicle, lamina, or facet joints that allows the front portion of the vertebra to slip forward with respect to the back portion of the vertebra.
● Pathologic spondylolisthesis: Pathologic spondylolisthesis is caused by a defect in the bone caused by abnormal bone, such as from a tumor.
What are the risk factors for spondylolisthesis?
Risk factors for spondylolisthesis include a family history of back problems. People who are born with a defect in the pars interarticularis bone in the spine (a condition called spondylolysis) are at increased risk of isthmic spondylolisthesis. Other risk factors include a history of repetitive trauma or hyperextension of the lower back or lumbar spine. Athletes such as gymnasts, weight lifters, and football linemen who have large forces applied to the spine during extension are at greater risk for developing isthmic spondylolisthesis.
What are spondylolisthesis symptoms?
The most common symptom of spondylolisthesis is lower back pain. This is often worse after exercise especially with extension of the lumbar spine. Other symptoms include tightness of the hamstrings, and stiffness and decreased range of motion of the lower back. Pain in the legs, thighs, and buttocks may worsen with standing. Some patients can develop pain, numbness, tingling, or weakness in the legs due to nerve compression. Severe compression of the nerves can cause loss of control of bowel or bladder function, or cauda equina syndrome.
What types of doctors treat spondylolisthesis?
Adiologists diagnose spondylolisthesis using X-rays, CAT scans, or MRI scans. Orthopedic surgeons, neurosurgeons specializing in the spine, physical medicine and rehabilitation doctors, neurologists, internists, primary-care providers, and rheumatologists commonly treat spondylolisthesis. Chiropractors and physical therapists also frequently treat patients with spondylolisthesis.
How do doctors diagnose spondylolisthesis?
How is the grading determined for spondylolisthesis?
Usually, it is not possible to see visible signs of spondylolisthesis by examining a patient. Patients typically have complaints of pain in the back with intermittent pain to the legs. Spondylolisthesis can often cause muscle spasms, or tightness in the hamstrings. The diagnosis of spondylolisthesis is easily made using plain radiographs. A lateral X-ray (from the side) will show if one of the vertebra has slipped forward compared to the adjacent vertebrae. Spondylolisthesis is graded according the percentage of slip of the vertebra compared to the neighboring vertebra.
● Grade I is a slip of upto 25%.
● Grade II is between 26%-50%.
● Grade III is between 51%-75%.
● Grade IV is between 76%-100%.
● Grade V, or spondyloptosis, occurs when the vertebra has completely fallen off the next vertebra.
If the patient has complaints of pain, numbness, tingling, or weakness in the legs, additional studies may be ordered. These symptoms could be caused by stenosis, or narrowing of the space for the nerve roots to the legs. A CT scan or MRI scan can help identify compression of the nerves associated with spondylolisthesis. Occasionally, a PET scan can help determine if the bone at the site of the defect is active. This can play a role in treatment options for spondylolisthesis as described below.
What is the treatment for spondylolisthesis?
What type of surgery treats spondylolisthesis?
The initial treatment for spondylolisthesis is conservative and based on the symptoms.
● A short period of rest or avoiding activities such as lifting and bending and athletics may help reduce symptoms.
● Physical therapy can help to increase range of motion of the lumbar spine and hamstrings as well as strengthen the core abdominal muscles.
● Anti-inflammatory medications can help reduce pain by decreasing the inflammation of the muscles and nerves.
● Patients with pain, numbness, and tingling in the legs may benefit from an epidural steroid (cortisone) injection.
● Patients with isthmic spondylolisthesis may benefit from a hyperextension brace. This extends the lumbar spine, bringing the two portions of the bone at the defect closer together, and may allow for healing to occur.
● Home remedies for spondylolisthesis are similar to those for low back pain and include ice, heat, and over-the-counter analgesics such as acetaminophen (Tylenol) and anti-inflammatory medications.
For those whose symptoms fail to improve with conservative treatment, surgery may be an option. The type of surgery is based on the type of spondylolisthesis. Patients with isthmic spondylolisthesis may benefit from a repair of the defective portion of the vertebra, or a pars repair. If an MRI scan or PET scan shows that the bone is active at the site of the defect, it is more likely to heal with a pars repair. This involves removing any scar tissue from the defect and placing some bone graft in the area followed by placement of screws across the defect.
If there are symptoms in the legs, the surgery may include a decompression to create more room for the exiting nerve roots. This is often combined with a fusion that may be performed either with or without screws to hold the bone together. In some cases, the vertebrae are moved back to the normal position prior to performing the fusion, and in others the vertebrae are fused where they are after the slip. There is some increased risk of injury to the nerve with moving the vertebra back to the normal position. Outcomes and recovery after surgery are improved with physical therapy rehabilitation.
What is the prognosis for spondylolisthesis?
The prognosis for patients with spondylolisthesis is good. Most patients respond well to a conservative treatment plan. For those with continued severe symptoms, surgery can help alleviate the leg symptoms by creating more space for the nerve roots. The back pain can be helped through a lumbar fusion.
Is it possible to prevent spondylolisthesis?
Spondylolisthesis cannot be completely prevented. Certain activities, such as gymnastics, weight-lifting, and football, are known to increase the stress on the vertebrae and increase the risk of developing spondylolisthesis.